PEPC One Pagers
PEPC one pagers spotlight the success of independent physicians and practices in CMS Innovation Center models and other shared savings programs, and highlight the role of value-based care in supporting and sustaining the independent physician workforce.

Studies & Reports

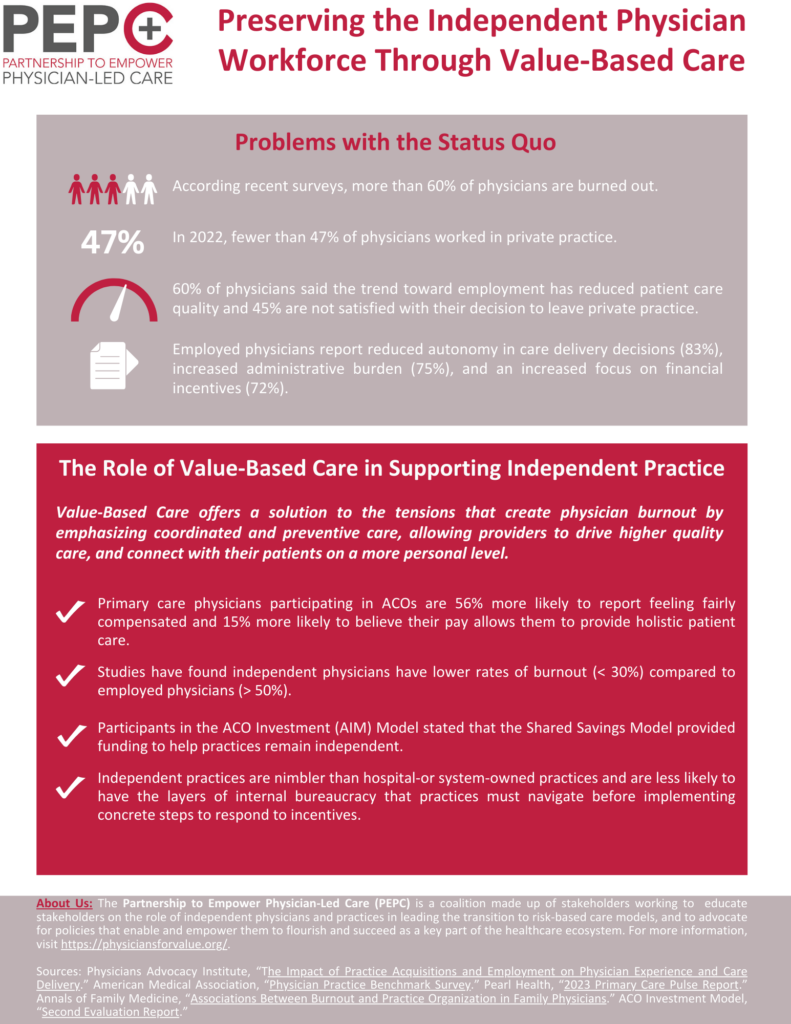
Why Physicians in ACOs Are Happier With Their Compensation: Primary care physicians who participate in an ACO were 56% more likely than non-ACO participants to believe they are paid fairly. ACO participants were also 15% more likely to believe that the way they generate revenue allows them to deliver holistic care.
About half of all physicians experience burnout. However, when studies are conducted of independent physicians specifically, that burnout level tends to be significantly lower. A limited study of independent primary care physicians published recently found that their burnout rate was only 13.5 percent.

Physician survey finds leaving private practice hurt patient care: Nearly 60% of physicians said the trend toward employment has reduced patient care quality, largely due to a lack of clinical autonomy and an increased focus on cost savings by facility leadership
“One of the key arguments for hospital mergers and practice acquisition was that health systems would deliver better-value care for patients. This study provides the most comprehensive evidence yet that this isn’t happening,” said author Beaulieu.

“Physicians significantly alter their care process after they vertically integrate,” Saghafian said. “This results in substantial increase in patients’ post-procedure complications.” Moreover, integration increased the number of patients a physician was able to treat and elevated reimbursement per procedure
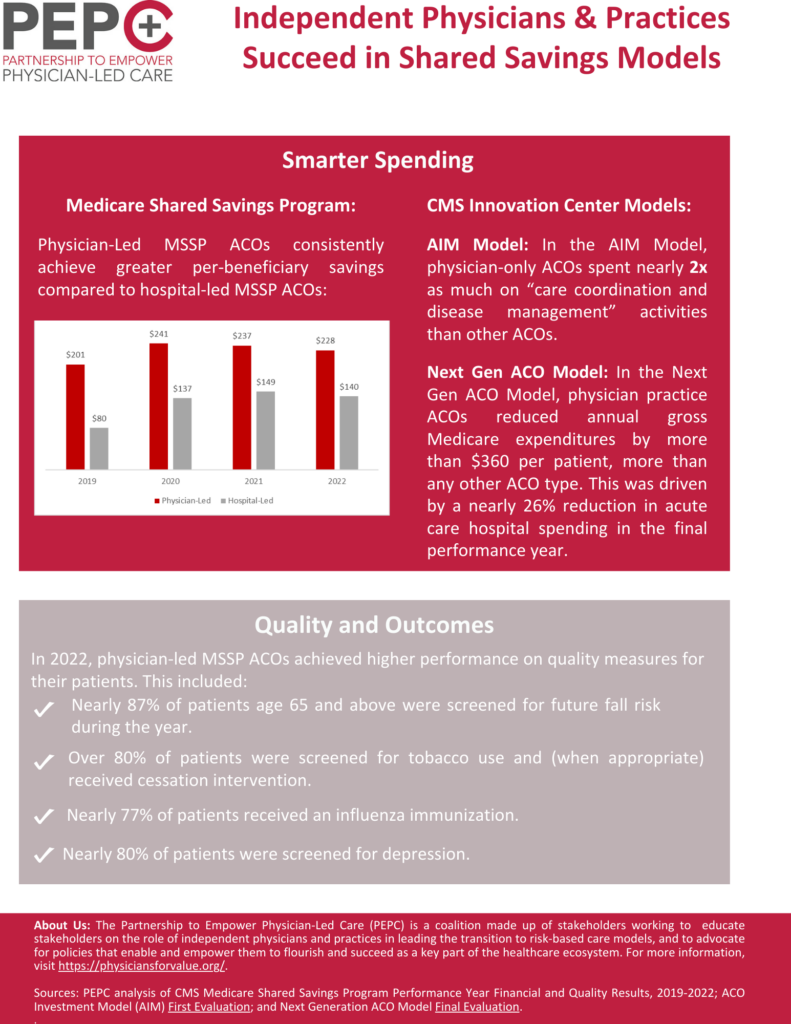
Physician-led accountable care organizations outperform hospital-led counterparts: On average, physician-led ACOs produced almost seven times the amount of Medicare savings per beneficiary than hospital-led ACOs.

Independent primary care physicians, because of their relationships with patients, are uniquely positioned to lead the transition to value-based care and succeed in new payment arrangements.

